Updated New Breastfeeding Protocol For Mastitis Treatment: How do I deal with an episode of Mastitis?
Share
CHANGES IN OUR UNDERSTANDING OF MASTITIS
The principle that mastitis is more about breast inflammation than milk stasis (clogged milk ducts)—or milk remaining in the breast when you skip feedings or your infant doesn't completely empty it—may be the most important lesson learned from the new protocol. Hyper lactation (Oversupply) or producing excessive amounts of milk is a factor, but it is not the primary cause.
ABM maintains that although mastitis frequently manifests as a bumpy, red, and sensitive patch in the breast that is referred to as a "plugged duct” or clogged duct, the actual reason isn't backed-up milk in one specific duct of the breast. Instead, overall breast inflammation causes the ducts to constrict, which produces breast soreness and redness on the breast. Sometimes your body display symptoms such as body aches, fever, chills, and tiredness in addition to just a sore spot in the breast. This condition is known as inflammatory mastitis, and with the right care it typically goes away on its own. Antibiotics are not needed to treat inflammatory mastitis. However, Bacterial mastitis is a rare infection of the breast that can occur. This indicates that bacteria—typically members of the Staphylococcus family—have infected the breast.
The red, painful area on the breast as well as the fever and chills are symptoms that are comparable to clogged ducts and inflammatory mastitis. ABM advises that you visit your doctor for a potential bacterial mastitis diagnosis if your temperature doesn't go down in roughly 24 hours. Bacterial Mastitis Antibiotics and probiotics can both be used to treat mastitis, though antibiotics are typically required. Bacterial mastitis does not require you to quit nursing and is not contagious. It will also not harm your baby. Additionally, if you have sterilised bottles or pumping components, advises against doing so.
PROTOCOLS FOR NEW MASTITIS TREATMENT
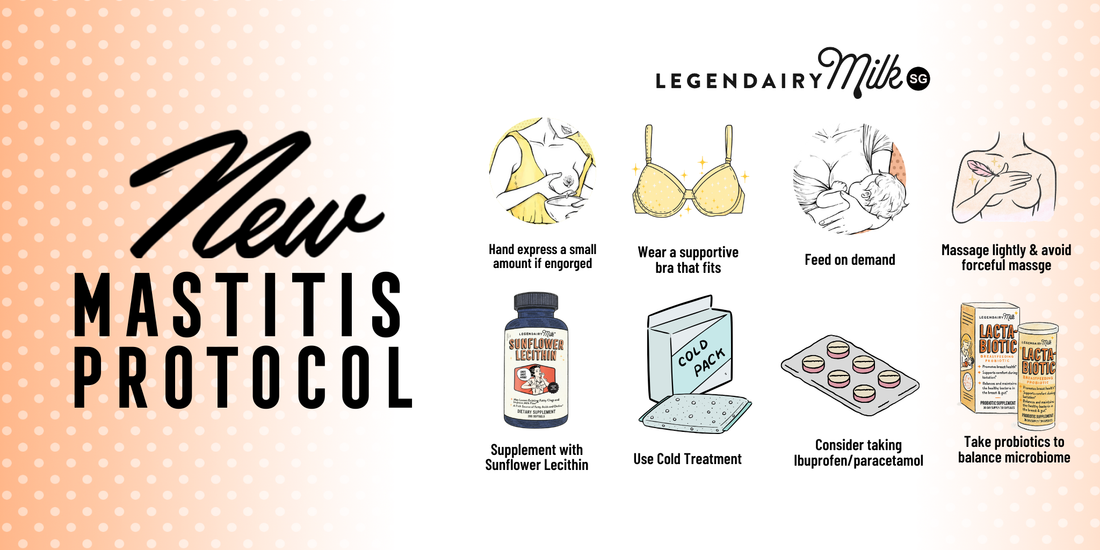
They now have a new knowledge of mastitis and a new set of suggestions for treating it. Here, reducing inflammation is more important than anything else. Do not do these anymore: Using forceful massage to break up a clog or unplug a duct Although you should still nurse when necessary, you should pump or nurse more to get the milk flowing.
Nursing on the swollen or blocked side, using massagers, electric toothbrushes, or other vibrating devices Epsom salt or castor oil soaks working out a plug in positions like "dangle nursing" What to do instead? Feed baby on demand and pump only when necessary as per schedule. Reduce inflammation between feeds using cold treatment. To relieve pain and reduce inflammation, take Ibuprofen/Panadol. You can hand express a small amount to soften the skin surrounding your areola if you are engorged and your baby is having trouble latching on. To reduce inflammation, using supplements with sunflower lecithin (5–10 grams per day are advised by ABM).
To balance your body's microbiome, think about taking Probiotics. To reduce hyperlactation (excessive milk production), breastfeed your child only when necessary and avoid pumping more than your child requires. Wear a supportive bra that fits properly if it's comfortable. If massage relieves your symptoms, go ahead and utilise it, but keep the pressure low and avoid deep massage.
HOW TO CONTINUE FROM HERE
Make sure to speak with a breastfeeding specialist or lactation consultant if you've tried all the remedies listed and you're still not feeling better. Here are a few crucial ideas to bear in mind: As previously said, if you have a fever for more than 24 hours, its best to see a doctor and get the right treatment plan, and its most likely bacterial mastitis which requires antibiotics.